Your heart labors in each and every second of every day to ensure that you are well and healthy. Since the development of heart diseases may go unnoticed, it is essential to be aware of what to look for at home. Home monitoring can assist you in being aware of changes, but professional diagnostic imaging offers you the correct determination you require to have peace of mind. The residents of Irving, TX, can receive a high level of heart scanning facilities at the community level. We will discuss what you can keep track of at home and under what circumstances a professional assessment is necessary.
Which are the most trustworthy at-home indicators that can be used to signify early heart disease?
Listening to the signals your body sends you can be used to spot possible heart issues in good time. Typical symptoms are unusual fatigue, which does not disappear after rest, dyspnea during routine activities, chest pain or pressure, and abnormal heart rhythm. Others observe that their legs or feet swell up. It could also be an indicator that something is wrong with the heart through dizziness or feeling lightheaded. Continued monitoring on blood pressure with an aid such as a blood pressure monitor will aid in tracking the progress. It is worth tracking consistent abnormal readings, especially elevated blood pressure, to identify potential concerns early. Nevertheless, such observations at home cannot cause self-diagnosis but professional examination. The services offered by ViaScan through heart scans are a source of detailed imaging, which will help properly evaluate cardiovascular health.
Important Symptoms to be monitored on a daily basis
- Abnormal tiredness or lack of strength in common activities.
- Puffiness when walking up stairs and walking.
- Pain, tightness, or pain in the chest.
- Feeling of abnormal or fast heartbeat.
- Ankle, foot and leg swelling.
- Constant lightheadedness or dizziness.
- Aching or soreness on the arms, jaw or back.
When Mild Signs Become Concerning
Sometimes tiredness or shortness of breath may not indicate serious illnesses, particularly when related to routine activity, but persistent or unusual symptoms should be assessed professionally. However, when such symptoms occur during rest or deteriorate in days or weeks, expert examination becomes relevant. In case the symptoms disrupt everyday life or appear in combination with several warning signs, it is better to schedule a heart scan and identify the cause so that the next steps could be taken.
What are the effective home-based tools that can be used to monitor heart health?
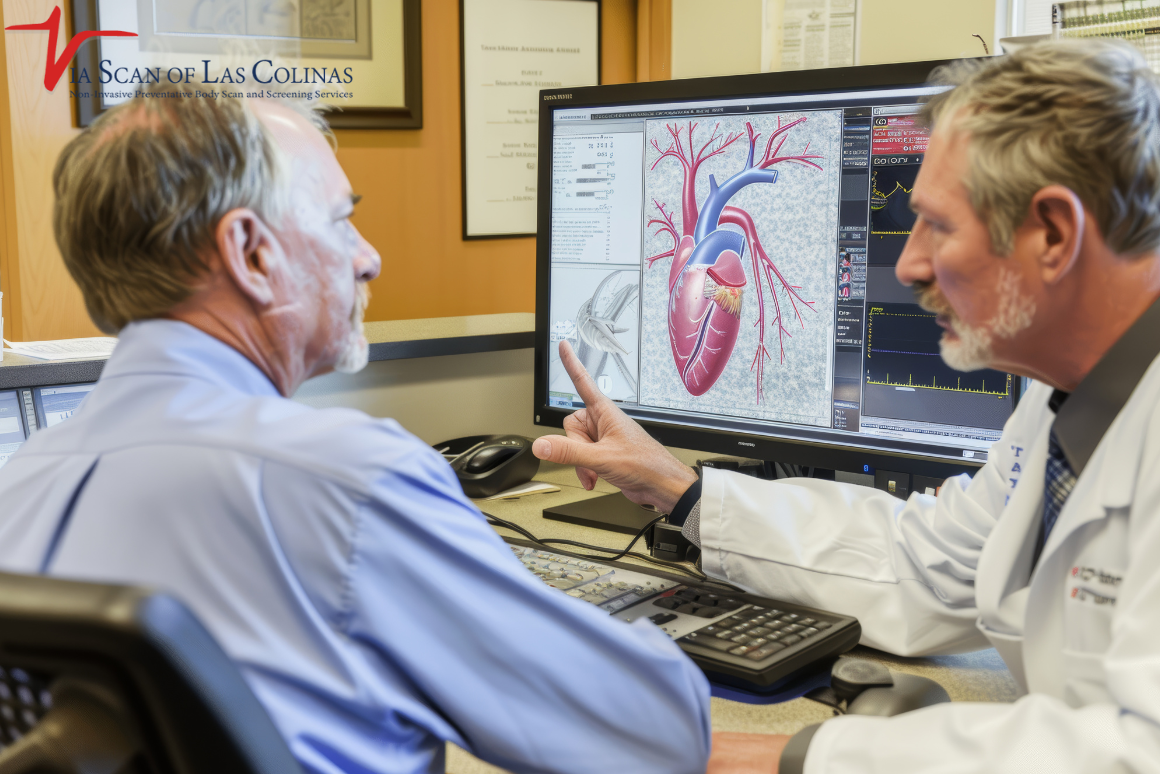
One of the most useful devices to use in heart monitoring at home is the blood pressure monitor. The gadgets record the pressure of the blood passing through your arteries. Monitoring your blood pressure aids in determining trends and fluctuations. Fitness trackers and smartwatch devices are able to measure heart rate during the day and night. There are gadgets that can monitor irregular heartbeats, though confirmation requires a professional evaluation. Pulse oximetry devices are devices that monitor oxygen levels in your blood. Though these tools are useful in their provision, they cannot substitute professional diagnostic imaging. ViaScan plans to provide CT scan and heart scan technology that can reveal details of heart structure and blood vessel health not detectable through home monitoring, used selectively based on risk factors.
Checking Heart Rate and Blood Pressure.
Frequent monitoring using a blood pressure device helps develop a normal level of your readings. Count every day, at about the same time in the morning before taking medicine or eating. Note both systolic (top figure) and diastolic (bottom figure). Keep an eye on such trends as a persistent increase in the numbers or consistently abnormal readings, which may reflect various cardiovascular issues. Provide these records to health professionals to evaluate them more thoroughly.
What role does lifestyle assessment play in the detection of early cardiovascular risk?
Examination of your daily habits is a valuable hint concerning the risk of heart disease. Your risk is high when there is a history of heart problems in your family. The development of cardiovascular disease is caused by smoking, high levels of stress, poor diet, and lack of exercise. Diabetes or being overweight, among others, impact the heart. Although these risk factors may not be causing you any trouble, they could be silently damaging your heart. A clear evaluation of the lifestyle factors can be used to define when it may be wise to conduct professional screening. The whole-body scan and heart scan service provided by ViaScan is able to identify early changes in blood vessels and heart tissue before symptoms manifest, particularly in patients who have several risk factors.
Determining Long-Term Risk Patterns.
The trend is more important than the cases. A single reading of high blood pressure following a stressful day is different to regular repeated readings of high blood pressure over a period of weeks. Likewise, any poor eating habits occasionally are not harmful compared to years of poor eating. Think of the length of existence of risk factors and whether they are progressing or not. This view can be used to emphasize the issues that require urgent specialist consideration.
What should at-home findings cause a medical evaluation?
Home monitoring is a preemptive system rather than a diagnostic tool. When your blood pressure monitor device continuously registers values that are not within normal ranges, then it is best to have them checked by a professional. The continuous symptoms that take more than several days must be considered. Emerging symptoms that slowly deteriorate need timely evaluation. Persistent abnormal readings or combinations of symptoms such as dizziness, unusual fatigue, or swelling should prompt professional evaluation. The ViaScan express CT scan has higher quality results showing blockages in the arteries, the calcium deposits and abnormalities in the structure which cannot be detected by home monitoring. Professional scanning helps to detect early and intervene in a timely manner before severe complications arise.
Cautionary Symptoms That Require Emergency Treatment
- Severe chest pain or pressure that is several minutes in duration.
- Sweating, nausea, and shortness of breath in the chest.
- The pain radiates to the jaw, neck, shoulders, and arms.
- Acute dyspnea.
- Dynoscopy or loss of consciousness.
- Rapid or extremely irregular heartbeat and dizziness.
When To Have a Professional Heart Scan.
In addition to emergency cases, there are some patterns, that may reveal the necessity to use the services of professional heart scanning. Constant symptoms without improvement should be evaluated. A combination of several risk factors such as family history, diabetes, and high blood pressure combined makes screening urgently needed. There is also the issue of age, men and women may discuss the possibility of baseline heart scans around 45 and 55 years of age with their doctor, especially when multiple risk factors exist. ViaScan offers convenient and high-quality heart imaging to the residents of Irving, TX with the concern of cardiovascular health.
Choose Our Preventive Heart Scan
Early Detection Saves Lives!
-
- Accurate
- Quick Result
- Affordable

conclusion
You need to be aware of the importance of protecting your heart health but professional diagnostic tools are necessary to measure it. Although the use of home monitoring tools, such as a blood pressure monitor, is beneficial in monitoring the changes every day and pointing to the red flags, it is only through further imaging, which is advanced, to see what is going on in your heart and blood vessels.
ViaScan is an organization in Irving, TX that deals with heart scans, CT scans, and whole-body scans that deliver a detailed heart analysis. Our state-of-the-art imaging techniques identify the symptoms of heart disease, blockage of the arteries, and calcium deposits that predispose to the risk. All the scans are examined by licensed radiologists in order to ensure proper interpretation of results.